The Respiratory System
Noah Greenspan, PT, DPT, CCS, EMT-B
KNOW THYSELF!
When it comes to dealing with a chronic illness, a basic understanding of the anatomy (structure), physiology (function) and pathophysiology (disease) will go a long way. My hope is that this information will help you better understand your condition, as well as provide you with the necessary vocabulary and context for more meaningful communication with your doctors and other health care professionals.
Breathing is “Multi-Factorial”
I tell people repeatedly that “breathing is a multi-factorial process.” What I mean by that is that on any given day, there are a whole host of factors, both internal and external to our bodies that can affect how well (or how poorly) we breathe. Besides just our lungs and the respiratory system, these can include things like proper medication use, activity versus inactivity, the foods we eat (or don’t eat), maintaining a healthy weight as compared to being overweight or underweight and managing stress and anxiety effectively; not to mention the possible effects of weather; and other environmental factors that can have either a positive or negative impact on our breathing.
As an example, think about how your body reacts when you step outside on a cold winter day as opposed to when it’s hot and humid; or how you feel after indulging in a big meal or having a few too many cocktails. Using temperature as an example, we know that our body functions best at a temperature of 98.6 degrees Fahrenheit. This is the reason why we sweat in the summer and shiver in the winter as our body attempts to cool and warm itself, respectively.
Breathing is Multi-Systemic
Breathing is also multi-systemic. Contrary to what many people believe, breathing is not just a function of the lungs and the respiratory system alone. In fact, multiple systems contribute to the act of breathing including the following:
- Neurologic system (brain, spinal cord, and nerves)
- Cardiovascular system (heart and circulation)
- Musculoskeletal system (muscles, bones, joints)
- Endocrine system (glands and hormones)
- Gastrointestinal system (digestion and the digestive tract)
- Hematopoietic System (blood and the production of blood cells)
While each system is specialized to perform a different function or set of functions, they are also interconnected, working together; constantly monitoring and adapting to changes in the internal and external environment to establish a physiologic state of balance known as equilibrium.
The net impact of each system will vary depending on the individual, and their condition and co-morbidities, i.e., other medical issues. Other systems can and will be involved on an individual, case-by-case basis. Therefore, it is essential that you, along with your doctor, investigate and explore all the factors that could potentially be contributing to your shortness of breath.
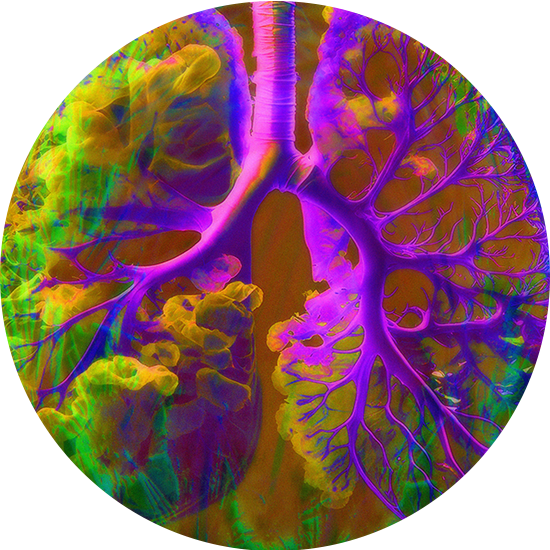
The Respiratory System
The primary functions of the respiratory system are to deliver oxygen (O2) to the body and remove carbon dioxide (CO2) and other waste products of metabolism. At the most basic level, when you take a breath, O2 molecules enter the lungs and cross into the bloodstream. This “oxygenated” blood is then transported to the heart, where it is pumped to every cell and organ of the body for use as fuel during metabolism.
CO2 and other metabolic waste products cross from the cells and organs of the body into the bloodstream. This “deoxygenated” blood is then transported back to the heart, where it is pumped to the lungs, where CO2 is expelled during exhalation.
Inhalation
Inhalation is an active process, meaning that it requires the active muscular contraction of the diaphragm, the primary muscle of inspiration (and the intercostal muscles) for it to occur. For us to take a breath, the brain sends a signal down the spinal cord to the phrenic nerve. When the phrenic nerve innervates (i.e., sends an impulse to) the diaphragm, it contracts downward, creating a negative pressure in the thoracic cavity. It is this negative pressure that causes the lungs to inflate, filling up with air.
When breathing demands increase—as in the case of physical activity or exertion, or in the context of respiratory disease, your body can call on the accessory muscles, which include the muscles of the neck, back, and chest, among others, to assist with ventilation.
People with restrictive lung diseases, such as Pulmonary Fibrosis and other ILD’s, typically have a difficult time with the inhalation phase of breathing due to increased stiffness of the lungs. As a result, they must generate significantly greater force in the respiratory muscles to overcome the increased lung resistance.
People with restrictive lung disease often take shallow breaths with less air in each inhalation. As a result, they are forced to breathe more rapidly to keep up with the body’s ventilation and respiration demands. This contrasts with people who have obstructive lung diseases (like COPD or Asthma), who have difficulty in expelling air out of the lungs.
Exhalation
During quiet breathing, exhalation is a mostly passive process, relying on relaxation of the respiratory muscles, and the natural elastic recoil of the lungs, which causes them to deflate and expel air. Exhalation can also become an active process when the expiratory muscles, particularly the abdominals, contract to actively force air out of the lungs. This forced exhalation can be done voluntarily or involuntarily and can occur during strenuous (or not so strenuous) activity, particularly in cases of impaired lung function.
People with obstructive lung diseases, such as COPD have a difficult time getting air out of the lungs during exhalation. This can be caused by several factors including airway inflammation, mucus or spasm in the airways, a decrease in the natural recoil in the lungs or the destruction of the small airways and alveoli. This contrasts with people with restrictive disease, who have increased recoil.
Ventilation and Respiration
The mechanical act of moving air in and out of the lungs, i.e., inhalation and exhalation, is called ventilation. Ventilation is an active process, meaning that it requires the contraction and relaxation of the respiratory muscles, for it to occur.
The chemical exchange of oxygen (O2) and carbon dioxide (CO2) between the external environment and the cells of the body is called respiration or gas exchange. Respiration is a passive process and occurs constantly, regardless of muscle activity or phase of ventilation. In other words, it occurs at the cellular level, during both inhalation and exhalation, as well as during any pauses in between.
While there are many factors involved in how well your body uses oxygen, its overall efficiency is based upon three main factors:
- How effectively your lungs move air in and out
- How effectively your heart pumps blood
- How efficiently your muscles utilize oxygen
If there is a problem in any one of these areas, your body will not be as efficient at using oxygen and you will be shorter of breath. For example, if you have a chronic respiratory disease, your lungs will not move air in and out as effectively. If you’ve had a myocardial infarction (heart attack), your heart will not pump blood as effectively. If you lead a sedentary lifestyle, then your muscles will not utilize oxygen as effectively.
If you have problems in more than one area (which is not uncommon), your breathing (and other issues) can multiply. As an example, if you have both heart and lung disease, you will likely have significantly more difficulty than if you had either one alone.
Here is the good news, though, and again, I am completely biased. But…in our experience, we have found that the right combination and type of exercise and breathing techniques can significantly improve the effectiveness of the respiratory, cardiovascular, and muscular systems, thereby improving your body’s overall efficiency at using oxygen.
Order Your Book Now!
Purchase Your Signed Copy Today!
- Within the United States: $27.50 including Postage and Handling!
- Outside of the US: $52.00 including Postage and Handling! (Sorry. We know that is more than the cost of the book but we cannot ship for less.)
Subscribe To Our Newsletter For Upcoming Offers
- Be the first to know about new webinars, exclusive offers, and podcasts.